Observations of a decade of low carb for T1D management. Has it been worth it? What are the regrets? And what has changed in that time.
Are Some People Just Lucky?
What are the two key elements of optimal diabetes management, and how can we ensure 'luck' is on our side? The answer is simple, but not easy.
Hypoglycemia Is Not The Goal
When people start optimizing blood sugar levels, many erroneously believe that lower numbers are always better.
Learn about hypoglycemia, where to set your alarms, how to find your hypoglycemia percentage, and why lower blood sugar is NOT better.
Food Prep for Fast Weeknight Meals
Melissa Joulwan's food prep plan changed my life nearly as much as Dr. Bernstein's Diabetes Solution did for diabetes.
Before I was ready to start Dr. Bernstein's plan, I tried everything else I could find.
One of those 'everythings' was the Whole30, which was such a valuable experience, I've done it a couple of times and wrote about why I think everyone should complete a Whole30 here.
While doing a Whole30 back in 2014, I read Melissa Joulwan's book Well Fed. The book is centered on Paleo eating, which has issues meshing with low carb in terms of the fruit content, but we'll ignore that right now.
Like Melissa says, I love cooking but I hate making dinner.
Dinnertime is inevitably the busiest time of day, with kids asking for help with homework, my husband telling me about his day, the doorbell ringing with deliveries, and it seems like a million other things going on.
Because of that, I keep dinnertime simple with meat and veggies. If those dinner ingredients are already prepped, you can save a ton of time and focus on more important things in your life (the people, of course!)
Melissa Joulwan teaches an amazing food prep Strategy that goes like this:
Buy groceries on Saturday (or whatever day works for you).
Plan Your prep day. The day of grocery shopping - or the day after - is usually best.
Spend an hour or so cooking up all the protein for the week. I often do this with only a couple of pans and just keep cycling one thing after another. Don't forget to boil eggs, too.
When cooled, store in containers in the fridge.
If needed, wash, chop and pre-cook your favorite fresh veggies for the week. Blanche, sautee, roast, etc. Okay, with lettuce and items eaten raw, just wash and chop. ;) Skip this with frozen or pre-prepped/bagged veggies.
Get your family involved so you can do together in half the time. Start some music, give everyone an age-appropriate task and you'll be done in no time - all the while with some great family bonding.
Then on your busy weeknights, grab a protein, grab a veggie - or a few - and….
Throw them together in a pan and add any type of spice mix you desire: Italian, Southwest, Asian.
Or add the meat and veggies into a pot with some coconut milk and curry spice to make a quick curry.
Or with broth to make a soup.
Or make a quick frittata by sauteing protein and veggies (asparagus, red pepper, etc) then add beaten eggs and bake until set.
Or make a hearty high-protein salad
The possibilities are endless and the thing is, you've just saved yourself an hour in the kitchen every evening.
Many people believe that home-cooked meals every night is an unattainable dream.
Or they think that they don't have time for a big meal prep once per week. But what if that 2 hours you spend on the weekend translates to 3 hours saved during the week when you need it most?
Melissa outlines this plan on her blog, plus includes links to a few of her favorite spice blends. (Keep in mind that the other recipes on this blog are Paleo/Whole30 and may or may not fit with Dr. B's low carb approach.)
*Two of our fav low carb spice blends are on the diaVerge blog: Magic Mushroom powder and Southwest Seasoning.
How will you use protein prep and the protein + vegetable + flavor concept to enhance your meal time? I’d love to hear what you think.
Do you have the Optimal Foods for Diabetes download?
It can help you get food planning/prep done faster and easier - and keep blood sugar levels on track.
It’s free and you can get it here.
Low carb, type 1 diabetes and pregnancy
Author: Lic.Lucía Feito Allonca, Heath Law and Biomedicine. Patient’s Rights Specialist. Diabetes Educator (DE)
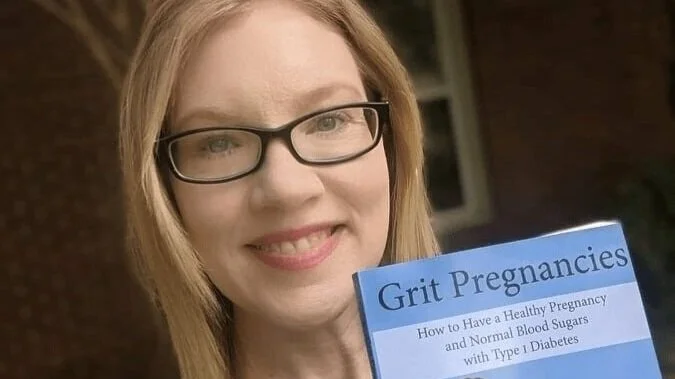
At International Low Carbohydrate Awareness Week 2023, Allison Herschede, BSN, RN, CDCES, gave a presentation on how to minimize risk in pregnancy for positive outcomes when living with diabetes.
Allison has been living with diabetes for 42 years, and was told to avoid pregnancy. However, she has had two successful pregnancies on the standard American diet - using high doses of insulin and having numerous episodes of severe hypoglycaemia - and one on the low-carbohydrate regimen, with normalised blood glucose levels and giving birth at 40 weeks. She has been leading pregnancy and diabetes groups since 2006 and is a registered nurse and diabetes educator. She has a book on this topic, available on Amazon, called "Grit pregnancies: How to have a healthy pregnancy and normal blood sugars with Type 1 Diabetes", available on Amazon.
THE RISKS OF TYPE 1 DIABETES IN PREGNANCY
In pregnancy with type 1 diabetes, the patient is at risk of miscarriage, birth defects and complications such as pre-eclampsia, progression of diabetic retinopathy, progression of chronic kidney disease, macrosomia (large for gestational age baby), too much amniotic fluid, neonatal hypoglycaemia, respiratory distress syndrome, jaundice, placental failure and, in the worst case, stillbirth.
As I anticipated at the beginning of the article, Allison has had three successful pregnancies, how to minimize these risks and their causes will be discussed below.
THE CAUSE OF THE RISKS
In terms of risk of miscarriage, pregnancy loss before 20 weeks gestation is more common in type 1 diabetes due to genetic abnormalities. Elevated fasting glucose is also closely related to the levels of maternal hormones needed to maintain pregnancy.
Birth defects occur mainly due to hyperglycemia. High blood glucose (sugar) levels during the first 10 weeks of gestation increase this risk.
For pre-eclampsia, macrosomia, placental failure, progression of diabetic retinopathy and diabetic kidney disease and other conditions, there is a common cause: again, these risks are caused by hyperglycemia
Dr. Lois Jovanovic-Peterson, an endocrinologist and pioneer in diabetes and pregnancy, states that "A fasting blood glucose level above 120 mg/dL in the first trimester increases the risk of macrosomia by 24%.
It is clear that hyperglycaemia or high blood glucose (sugar) levels are the cause, not type 1 diabetes per se, if properly and strictly managed, which is in our interest to do at such a special time in our lives.
RISK MINIMIZATION STRATEGIES
The levels "in range" during pregnancy are as follows:
As of 2023,the ADA recommends a fasting blood glucose level of 70
As we have seen before, hyperglycaemia is the cause behind all the risks, and to avoid it, normalising our blood glucose or blood sugar values is essential. Is this possible
Yes, it is. Allison is a coach for diaVerge diabetes and has been helping people for many years to optimise the management of their type 1 diabetes and improve their time in range and glucose results.
Some tips for normalizing our glucose levels are as follows:
Therapeutic restriction of ingested carbohydrates: avoid cereals, sugar, starches and sweet fruit.
Test basal insulin. Find our ideal dose.
Test our insulin and glucose sensitivity.
Implement the use of regular insulin or give extended boluses to cover protein in the diet.
The use of continuous glucose monitoring (CGM).
Dr. Richard Bernstein, who has been living with type 1 diabetes since 1946 and still practices medicine, is convinced that people living with diabetes have the right to enjoy the same blood sugar levels as people without diabetes, and has provided us with his protocols and findings in his best-selling book "Diabetes Solution".
His method differs from the predominant recommendations on the global scene. Bernstein stresses that diabetes is a condition of carbohydrate intolerance, and that lowering insulin levels by eating fewer carbohydrates makes managing our diabetes a more predictable task.
As far as calories are concerned, in pregnancy we need to consider an extra 200-400 calories more than usual, 400 during the third trimester, taking into account that fat provides 9 calories per gram and protein 4 per gram, a packet of nuts contains 500 calories, so this increase will not be a difficult target to meet.
If done consciously, a low-carbohydrate eating plan can provide all the necessary nutrients. It is especially recommended to increase the intake of foods rich in folic acid (such as liver, peanuts, almonds or hazelnuts).
On the other hand, a low-carbohydrate diet can lead to nutritional ketosis, not to be confused with diabetic ketoacidosis. Nutritional ketosis is a natural state, whereas diabetic ketoacidosis is an acute and life-threatening complication of diabetes.
Basal insulin requirements may change in pregnancy and it is important to monitor them. The use of glucose tablets or similar is recommended to dose the amount of carbohydrate with which we treat potential hypoglycemias, as food is much less predictable.
Overeating, Binge Tendencies, Insatiable Appetite?
For those of us navigating the tricky landscape of type 1 diabetes, hunger is often more than just a passing craving — it can be an everyday challenge.
The truth is, it's not your fault. You are not lacking willpower. You are not lazy. You are NOT to blame.
There are very specific physiological reasons why you may feel hungry all the time. From fluctuating blood sugar levels to the complex dance of hormones, there are numerous reasons why relentless hunger pangs often accompany life with T1D.
What are these reasons and what can we do about it?
Polyphagia is the medical term for increased appetite, and there are both medical and non-medical reasons for this:
People with T1D do not produce amylin. Amylin is hormone that is co-secreted with insulin by the pancreatic beta-cells in response to food consumption. Since beta cells are destroyed or damaged in T1D, amylin is also not produced. Amylin’s role is a physiological control of meal-ending satiation (feeling full), and it limits the rate of gastric emptying, and reduces the secretion of pancreatic glucagon after eating. So, amylin tells you when you’re full, keeps food in the digestive tract for longer, increasing nutrient absorption, and helps to control blood sugar spikes after eating. And we don’t have this incredible helper hormone. Great (eyeroll).
Hyperthyroid/Graves disease can increase hunger levels, causing overeating.
Sleep deprivation/interruption - Acute sleep deprivation reduces blood concentrations of the satiety hormone leptin. Leptin sends a signal to your brain that helps you feel full and less interested in food. It also plays a role in how your body turns fat into energy. Sleep deprivation also increases the hormone ghrelin, which signals hunger. This is the perfect storm to make you feel hungrier, and less full/satisfied once you eat.
Growth hormones in kids: this is normal, and usually causes times of increased appetite, followed by an obvious growth spurt.
Estrogen in women: Increased appetite is due to spikes in the hormones estrogen and progesterone, and decreased levels of serotonin, which is a neurotransmitter. Decreases in estrogen (perimenopause & menopause) can cause both increased hunger cues and insulin resistance.
Low testosterone in men is associated with dysregulated eating
Nutrient and electrolyte deficiencies: Deficiencies in iron, Vitamin D, and B Vitamins all can cause increased hunger because your body is seeking those vitamins. Request these tests at your next lab blood draw and follow your doctor’s advice to supplement, if needed.
Blood sugar levels:
Hypoglycemia/low blood sugar levels cause a very real need to eat, and it’s our body’s method of self-preservation. We need to eat to raise our blood sugar level to stay alive! Oral liquid glucose or glucose gel, or glucagon treatment is the fastest way to raise blood sugar levels quickly and stop this insatiable need to eat.
Hyperglycemia/high blood sugar levels can also cause an increased appetite because without insulin, the body cannot process the food consumed into energy, thus craving more.
Processed Food Addiction: Processed foods are engineered to be addictive, keeping you craving and buying more. Dr. Joan Ifland is a leader in processed food addiction research and treatment. She advocates for a whole foods diet, and removal of all processed trigger foods from your surroundings. You can find out more about her program at foodaddictionreset.com
Complex relationship w/ food. Of course, we need food to live, but food raises our blood sugar and requires insulin. Because of this, many of the reasons above, and common diet culture, many people with type 1 have struggled with their weight and their relationship with food. It’s a complex issue, with many interconnected factors.
But what can you do about all of this? Is there a way out?
Be kind to yourself.
Talk to your doctor.
And consider increasing your protein consumption percentage.
We know that protein will keep you full for longer than carbs or fat will, that’s purely because protein foods take longer to break down in the digestive system, and per gram of food, protein foods have more nutrient density and calories than carbs or fat.
Because of this nutrient and energy density, the Protein Leverage Hypothesis states that the body craves protein for survival, and will eat until the optimal protein threshold is reached. If not enough protein is consumed, it will continue craving, and eating whatever it can to reach that protein threshold.
This protein threshold is helpful, because by prioritizing your overall protein percentage, you effectively leave little room for carbs in the diet, and consume fewer calories overall to get to that protein threshold.
Other things you can do:
Synthetic amylin replacement (called pramlintide, brand name Symlin) is available, but it has challenges to use and is rarely prescribed.
Sugar-free electrolyte supplementation is helpful, and adequate sleep (7+ hours) is a must when it comes to helping regulate the complex interplay of hormones.
If constant hunger, overeating or binge tendencies are an issue for you, please know that you’re not alone. This is a complex issue that many of us experience daily. Let’s normalize this as a part of life with type 1.
What is diabetes? Types of diabetes
Written by Lucía Feito Allonca, Heath Law and Biomedicine. Patient’s Rights Specialist. Diabetes Educator.
There is a lot of talk about diabetes, but what is it really?
Is it a single health condition, or several?
Are there different causes for developing diabetes, or are there common elements?
With the aim of disseminating reliable information and education on diabetes, I attach this article that I wrote within the framework of the “This IS diabetes” campaign in Beyond Type 1, with the aim of eradicating myths and erroneous beliefs, harmful to our health.
The Latin phrase diabetes “to pass through” comes from the Greek loan word Dia “through” and Betes “to pass.” It is, according to the dictionary of the Royal Spanish Academy, a metabolic disease characterized by excessive urine output, weight loss, intense thirst and other general disorders.
TYPE 1 DIABETES
Type 1 diabetes was previously also known as juvenile diabetes due to the high number of diagnoses in children and young people. Today it is known that type 1 diabetes can appear at any time of life, not just childhood or adolescence.
It is a chronic condition of autoimmune origin that causes the body to be unable to produce the hormone insulin, responsible for regulating blood glucose (sugar) levels. Its symptoms are polyuria, which means frequent urination, polyphagia, which implies excessive hunger, weight loss that occurs without apparent explanation, and tiredness/fatigue.
It is important that we understand that type 1 diabetes has an autoimmune origin and that the person will depend on the external supply of the hormone insulin to live and stay healthy.
It is essential to put an end to myths and erroneous beliefs that still circulate in society, such as that “diabetes is a thing for older people” or that “insulin is for serious cases.” In type 1 diabetes, insulin is the only treatment option.
Managing type 1 diabetes involves making interventions in people's lifestyles, such as diet, exercise, and taking insulin. To carry out an adequate dosage of this hormone we must know our blood glucose (sugar) levels, a task which will require a continuous glucose meter or blood glucose measurements made with a blood sugar meter. The success of treatment will be affected by the level of commitment of the family and the environment, personal/family circumstances, as well as other socio-economic factors.
TYPE 2 DIABETES
Diabetes 2 manifests itself when the body cannot use insulin adequately, presenting the so-called “insulin resistance.” The pancreas releases extra insulin, but over time it can't keep up with production to keep blood glucose (sugar) levels in a healthy range.
The factors that influence the appearance of type 2 diabetes are obesity, smoking, genetic factors and factors related to lifestyle, making it a multifactorial condition.
The myths that single out and stigmatize people who live with type 2 diabetes often do so because they do not understand the cause of the disease.
Also, the use of insulin seems to be associated in popular culture with negative connotations, something that we have to tackle at its roots, since allowing these erroneous beliefs has a serious associated cost: posing a psychological obstacle for many people who need it to be able to take insulin, enjoy better health and quality of life.
GESTATIONAL DIABETES
It is a type of diabetes that causes high blood glucose levels during pregnancy. It usually starts between the 13th and 28th week of the pregnancy and will disappear after the baby is born.
Gestational diabetes causes a high level of blood glucose, dangerous for your baby's health, and subsequently produces a greater risk of type 2 diabetes in the future.
LADA DIABETES
Like type 1 diabetes, Latent Autoimmune Diabetes in Adults (LADA) is the result of an autoimmune process. This type of diabetes usually occurs in people over 30 years of age, which is why it is often misdiagnosed as type 2 diabetes.
MONOGENIC DIABETES (MODY)
Monogenic diabetes (MODY) is a type of diabetes that has characteristics of type 2 diabetes and occurs at a young age, usually before the age of 25.
It is due to mutations in certain genes (there are 7 known gene mutations at this time that cause MODY) and in a single gene subtype that affects the maturation of pancreatic beta cells (insulin-producing cells) and therefore, insulin secretion. It is a type of diabetes that is frequently misdiagnosed as type 1 or type 2 diabetes.
TYPE 3C DIABETES
It is related to pancreatic diseases such as pancreatitis (of which the most common causes are gallstones or alcohol abuse), pancreatic cancer, cystic fibrosis, pancreatic surgery and hemochromatosis.
Chronic pancreatitis is the most common cause and is often misdiagnosed as Type 2 diabetes.
Even with these various types of diabetes, and a variety of medications/technologies available for management of the condition, we are more alike than we are different. We ALL have issues controlling blood sugar level. As noted above, the lines between the types are often blurry and easily confused by medical professionals, patients, and the general public.
Let’s spread awareness, understanding, and compassion for all people who are impacted by diabetes, of all types.
Did you know of all the different types of diabetes? Leave a comment below to share!
Addiction, Processed Food & Diabetes - with Dr. Joan Ifland
Processed food addiction is common, and can be a barrier for those with diabetes who want to gain control of blood sugar levels and weight. Lucy of diaVerge Diabetes interviews Dr. Joan Ifland, expert in processed food addiction here.
The Gap Between Knowing & Doing
Are you a person who knows what you should do and does it? Or are you a person who gets lost in the details or procrastination, and never takes the steps to do what you want to do?
Low Carb Diets, Children, Adolescents, and Technology
by Lucía Feito Allonca
In this post I will discuss two recent studies on the treatment of diabetes with a low carbohydrate diet.
Firstly, a study by the Spanish Diabetes Society where the conclusion was clear: that low-carbohydrate eating coupled with the use of technology is beneficial for diabetes management, and secondly, a recent study on low-carbohydrate diets in children and adolescents living with or at risk of developing diabetes.
Low carb diet + Closed Loop Systems: Better glucose management
In a recent study conducted by the Spanish Society of Diabetes (SED), it was found that even though up to 66% of patients with type 1 diabetes (T1D) were following a diet considered balanced, only a third of them were able to maintain an HbA1c level below 7%. Additionally, around 40% of T1D patients were overweight or obese. This raises the question of whether the conventional diet recommended for these patients is the most suitable and whether there are alternatives to achieve better therapeutic outcomes.
In the 2020 update of the American Diabetes Association (ADA) guidelines, low-carbohydrate diets were included as one of the healthy dietary options.
In T1D patients using closed-loop insulin infusion systems (hybrid closed-loop systems), it has been observed in a retrospective observational study at the Vall d’Hebron Hospital in Barcelona that combining a low-carb diet with this technology can lead to more stable blood sugar control, especially during the night when there are fewer external stimuli.
Low Carb Diets in Children and Adolescents with or at risk of diabetes
The present study is very recent and dates from 18 September 2023. It examines the use of a low-carbohydrate diet as a tool for weight loss and management of type 1 and type 2 diabetes.
It highlights the fact that the pediatric population in the United States faces a serious problem: obesity, and that its prevalence is increasing. It is noted that low-carbohydrate diets have been used for decades in adults to improve metabolic health and treat diabetes.
Current dietary recommendations for children and adolescents with type 1 diabetes reflect those of the general population. It is common to dose insulin at mealtimes according to the amount of carbohydrate to be eaten. People with type 1 diabetes may use low-carbohydrate diets to facilitate the reduction of exogenous insulin requirements and reduce mealtime blood glucose excursions.
However, although we are aware of success stories, there are very few data on the use of very low-carbohydrate or ketogenic diets in children and adolescents with type 1 diabetes. A study in adults with type 1 diabetes showed a decrease in insulin requirements.
A survey was conducted with an international social network-based group of adults with type 1 diabetes and parents of young people with type 1 diabetes who choose to use low or very low carbohydrate diets as an adjunctive treatment. Respondents reported excellent glycaemic control, but a poor relationship with diabetes professionals associated with mistrust and a feeling of being judged for their diabetes management decisions.
The study notes that there is clinical consensus to support lower carbohydrate intake and higher quality protein and fat intake in young people under medical supervision, if this is their choice and they have family and medical support, open dialogue about diabetes management decisions, dietary habits and choices, and regular medical follow-up with a supportive multidisciplinary team, including a pediatric dietitian.
Type 2 diabetes results from resistance to the physiological action of insulin in muscle and liver and progressive failure of pancreatic β-cells leading to relative insulin deficiency. Treatment requires addressing insulin resistance and insulin deficiency. Reducing carbohydrate can be an important and effective part of the overall management of type 2 diabetes, as it reduces insulin resistance and the demand for increasing amounts of insulin by the pancreas. As with people with type 1 diabetes, people with type 2 diabetes who use exogenous insulin for treatment can follow low-carbohydrate diets to lower blood glucose values and reduce exogenous insulin requirements.
Moderate or low-carbohydrate diets in adults with type 2 diabetes are beneficial for blood glucose and cardiovascular disease risk.
The final conclusions are as follows:
Low-carbohydrate (<26% energy) and very low-carbohydrate (20-50g) diets are not recommended for children and adolescents with type 1 diabetes, except under close supervision of a diabetes care team.
For the prevention and treatment of pre-diabetes and type 2 diabetes, it is recommended to reduce intake of nutrient-poor carbohydrates by minimising consumption of processed foods with large amounts of refined grains and added sugars and eliminating sugar-sweetened beverages.
Eliminating sugary drinks and juices significantly improves blood glucose and weight control in children and adolescents.
Although the recent news headline "Low-carbohydrate diets are not recommended for children" is often published, it does not tell the whole story.
It is still possible for us as a family to decide that a diet that reduces carbohydrate intake is the approach we want to take to avoid dangerous glycaemic excursions in our children and adolescents.
With the supervision of our health care team, and regular check-ups, we can arrive at the diabetes management outcomes we want, for ourselves and our loved ones.
Welcome Lucy! Bienvenida a Lucía!
Welcome to our newest diabetes educator, Lucia Feito Allonca! Lucy is a lawyer in Health Law, Bioethics & Patient Rights, and is holds a Diabetes Educator Certificate through IDF. She’s also lived with type 1 diabetes for more than 30 years. Lucy is providing type 1 diabetes education for optimal blood sugar management in Spanish.
Beat The Heat: Hot Weather Protocol for People Using Insulin
Do you know how to keep yourself - and your insulin - safe in extreme hot temperatures? Click here to read all about what you can do as a person with diabetes to have a fun, active summer AND stay safe.
Bolus Insulin Problem-Solving Guide
FREE DOWNLOAD: Problem-solving guide to bolus/mealtime insulin. Figure out what's happening and how to solve it with this handy downloadable guide to blood sugar levels and glucose corrections.
Your Future Self Will Thank You
Founder of diaVerge Featured in Nasdaq!
Disrupting the standards… and the outcomes
diaVerge is disrupting the mediocre standards of diabetes education and helping people with type 1 diabetes achieve huge improvements in blood sugar, weight, blood pressure, and other health markers.
What Knitting a Sweater Teaches About Habits - and Diabetes Management
by Lisa La Nasa, founder of diaVerge Diabetes
It’s time for New Year's goals and resolutions.
Today, I'm pulling back the curtain and showing you more about my life outside of diabetes management and social media.
Here's something you may not know about me:
I love textiles and fiber arts.
Sewing is my first love, and comes more naturally to me.
Knitting, though, has been an enigma (a mysterious, difficult, frustration) that I really want to change.
After 15 years of years trying to knit, with small projects here and there, sometimes finishing, sometimes not, I've decided that 2023 is my year to really get good at knitting.
I'm committed to honing my skills and I’m dedicating the necessary time to do so.
Lisa with a ball of yarn and new knitting set - and an unedited, unusually elongated head 🤣
In fact, I have a brand new set of knitting needles that I received for Christmas (thanks, Mom!), and I'm finally using up some wild multicolor yarn that I've had in my office/craft closet for the last 2 years.
Since I've knitted small projects previously but haven't been consistent with it, I have to start over each time and re-learn what I’ve forgotten.
I'm going for the gusto this time. No more taking years off and then expecting to pick it back up again. I'm going for something that I have to devote the time and effort to complete, that is a challenge and will build my skills.
I’m knitting a sweater.
This will take many weeks, and I need to devote the time every single day to get it done. To ensure this happens, I've scheduled it in my calendar. There’s a block of time every day for knitting.
This is not just a hobby. It's personal development.
It's learning and mastering a new skill.
It’s being comfortable with the discomfort of being a beginner.
It's practicing and learning from missteps.
It's building consistency and doing it every day whether I feel like it or not.
And that's exactly what we need to do to build new habits and skills.
The bottom ribbing of my new sweater.
Plus, it’s setting an example of commitment and follow-through for my 10-year-old daughter who also wants to knit.
AND, it’s quality time as we chat while we knit together.
Diabetes management is also a skill — but it’s one that we don’t often think of in the same way.
As a result, this is not something that most people devote the time to mastering.
Even though we might have been practicing diabetes management for years, most of us only learn bits and pieces, then wonder why we’re not achieving the same results as people on the internet who make it look so easy. But that’s not fair for anyone because we’re comparing our starting point to others mastery.
The truth is, it’s rare that people with type 1 will ever dedicate the time needed to improved diabetes management.
If you’re one of those few, and improved health (and diabetes management) is on your goal list for 2023, start here:
Commit to making improved diabetes management a daily practice
Read Dr. Bernstein’s Diabetes Solution book. If you’ve already read it, read it again. ;)
Schedule time in your calendar DAILY for learning and putting information into action.
Review your data OFTEN (using Dexcom Clarity, Libreview or other program of your choice)
Adjust your inputs when needed (quantity and/or timing food, insulin & exercise)
Seek out help such as an accountability partner who can give you a friendly nudge and help along the way when you don’t feel like doing the work
We all have the power to see what parts of our lives may need attention, and focus our efforts on learning and growth.
It requires commitment, time, and focused action to make improvements. Just don’t leave your future up to chance.
If you want to skip past many of the learning steps (and potential missteps) or you know you need accountability, structure and professional guidance along the path to improved health and habit formation, we can help.
diaVerge offers customized 1:1 coaching options and our flagship Diabetes Redesigned Membership (where you’ll get lifetime support and a Success Guarantee).
If you’re ready to build the habits of improved diabetes management, schedule a no-pressure call with me so I can learn more about you, your experiences with diabetes, and what might best help you reach your goals.
We're DCB Open Innovation Semifinalists!
diaVerge is working to develop the future of diabetes education through the intersection of personal connection, compassionate support, and technology.
This past August, the diaVerge team, lead by Lisa La Nasa and Pat Rowe, applied to the Diabetes Center Berne (DCB) International Open Innovation Challenge for our proprietary type 1 tech solution and we were thrilled to be announced as Top 20 Semifinalist in September.
As semifinalists, we received mentorship from global leaders specializing in diabetes, tech, funding, and legal/regulatory considerations, many with T1D themselves.
The process of application, refining our proposal, and meeting with this group of mentors was an incredible experience that pushed us as a team to explore the 'why' and 'how' of optimal diabetes management, and what can be done to bring compassionate diabetes support & education to those with type 1 worldwide.
Although diaVerge didn’t make the final 3, we’re incredibly happy for the teams who did. There were many well-developed, deserving proposals, but the final 3 really stood out as exceptional.
It was an honor to be among the top 20 semifinalists, and we're grateful to DCB and all of our advisors and mentors who have helped us along the way.
This is not over, though! We're applying to other think tanks, innovation challenges, and tech accelerator opportunities. The past three months have pushed us to see what is possible - and sorely needed within the T1D community - and we're just getting started!
Stay tuned for more.
Patrick Rowe joins the diaVerge Team
10 Tips for Low Carb Success
If you’re new to diabetes, or want to improve your diabetes management using a low carb approach, these are the top 10 steps you should take to get started.